Study Bay Coursework Assignment Writing Help
Introduction:
Clostridium difficile is the most common cause of health care associated infection and is almost always restricted to infection of the colonic mucosa. Small bowel involvement of clostridium difficile infection is extremely rare. We describe a patient with community acquired clostridium difficile associated enteritis. Management involves early diagnosis, intravenous hydration, aggressive therapy with antibiotics and supportive care to avoid the high mortality and morbidity associated with Clostridium difficile enteritis.
Case Report:
22-year-old female with past history of uncontrolled type I Diabetes mellitus (Hemoglobin A1C 9.9%), non compliant with medications, presented to the emergency department, with chief complaint of worsening abdominal pain associated with nausea and vomiting for 3 days. She described her abdominal pain as sudden in onset, dull, constant, about 5/10 in intensity and associated with nausea and 4-5 episodes of non bloodyvomiting since the past 3 days. She was frequently eating hamburgers and sausage biscuits at fast food joints. She denied any fever, chills, hematemesis, hematochezia, melena, sick contact, antibiotic use or recent hospitalization. Her examination was remarkable for hypoactive bowel sounds and periumblical tenderness on deep palpation. CT scan of the abdomen on admission showed ileus with small bowel wall thickening concerning for enteritis (See figure series A). Admission labs were remarkable for white blood cell count of 14.3 k/mm3, with 85% neutrophils, Glucose 205 mg/dL, and an ESR and C reactive protein being 76 mm/hr and 380 mg/Lrespectively. Stool Clostridium difficile toxin PCR was positive. The stool sample collected was near solid in consistency.A diagnosis of Clostridium difficile associated enteritis was made, and the patient was started on oral metronidazole 500mg three times a day. Her symptoms of abdominal pain improved and after 5 days of therapy her oral intake was better and a repeat CT scan showed interval improvement in small bowel thickening (See figure series B).


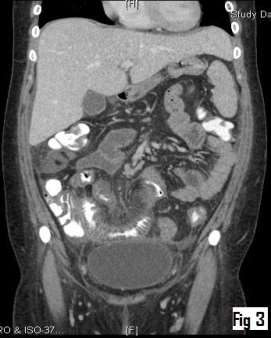

Fig series A: CT abdomen with contrast showing longitudinal sections of the abdominal cavity. (Fig 1 to 4 demonstrate anterior to posterior cut sections). Thickening of the small bowel in the right lower quadrant consistent with inflammatory changes was observed. No colonic involvement was observed.




Figure series B: Repeat CT scan done 5 days later on oral metronidazole therapy, showed interval improvement in the small bowel thickening. Again Fig 1 to 4 demonstrates anterior to posterior longitudinal sections of the abdominal cavity.
Discussion:
Clostridium difficile is an anaerobic gram-positive, spore-forming, toxin-producing bacillus. Clostridium difficile associated diarrhea from colitis is a very common entity due to increased use of antibiotics. Enteritis from Clostridium difficile is very rare. Our patient developed Clostridium difficile enteritis as a community acquired infection. She never used any antibiotics in the past and the reason for her to develop enteritis was unclear. Although we postulate that the patient had developed gastro paresis from herlong standing uncontrolled Diabetes. Reduced gastric acid secretion (1) and consumption of meat products (2) have been associated with increased risk of C.diff infection. Our patient had small bowel thickening on CT scan (see image series A) with positive C.diff in the stools. She slowly improved with metronidazole 500 mg thrice daily. A repeat CT scan 5 days later (See image series B), showed improvement in small bowel thickening. The patient’s abdominal pain also resolved. The patient was subsequently discharged home, with recommendations to follow up with gastroenterology for work up of possible inflammatory bowel disease predisposing to her enteritis, but she was lost to follow up and her underlying risk factors could not be assessed.
Based on the literature analysis done by Dineen et al, there have been a total of 83 cases reported so far (3). Frieler et al in 2001 reported a total of 9 cases that had occurred prior to 2001 (4). A total of 74 cases since 2001 have been reported. We are not sure whether the increase in the number of cases is due to increased incidence or increased detection. Most of the enteritis cases that have been reported in the literature generally have had underlying co-morbidities like crohns, ulcerative colitis or colon cancer (5, 9, 12). Williams et al and Peacock et al in their reports describe patients with ileostomy after colectomy that had developed Clostridium difficile enteritis (6, 7).C. difficilesmall bowel enteritis may be associated with a higher case-fatality rate than that reported withC. difficilecolitis due to secondary enteric necrosis and perforation. (1).Early diagnosis of disease by imaging and toxin detection is of paramount importance in improving outcomes.
PATHOGENESIS OF C DIFF ENTERITIS
Risk factors
 (Antibiotics, recent hospitalization, use of chemotherapy agents, inflammatory bowel disease)
(Antibiotics, recent hospitalization, use of chemotherapy agents, inflammatory bowel disease)
 Disruption of enteral microflora
Disruption of enteral microflora
 Clostridium difficile colonization
Clostridium difficile colonization
 Toxin A (enterotoxin) and toxin B (cytotoxin) release
Toxin A (enterotoxin) and toxin B (cytotoxin) release
Mucosal injury and inflammation
References:
1. Clostridium difficile induced necrotizing enteritis. Wiggelinkhuizen M1,Gerrits MA. Ned TijdschrGeneeskd.2011;155(49):A2414.
2. Dial S, Delaney JA, Barkun AN, Suissa S. Use of gastric acid-suppressive agents and the risk of community-acquired Clostridium difficile-associated disease. JAMA. 2005;294:2989–2995.
3. Dineen SP1, Bailey SH, Pham TH, Huerta S. Clostridium difficile enteritis: A report of two cases and systematic literature review.World J Gastrointest Surg. 2013 Mar 27;5(3):37-42.
4. J. Glenn Songer,corresponding author Hien T. Trinh, George E. Killgore, Angela D. Thompson, L. Clifford McDonald, and Brandi M. Limbago. Clostridium difficile in Retail Meat Products, USA, 2007.Emerg Infect Dis. May 2009; 15(5): 819–821.
5. Freiler JF, Durning SJ, Ender PT. Clostridium difficile small bowel enteritis occurring after total colectomy.Clin Infect Dis. 2001 Oct 15;33(8):1429-31
6. Williams RN1, Hemingway D, Miller AS.Enteral Clostridium difficile, an emerging cause for high-output ileostomy.JClinPathol. 2009 Oct;62(10):951-3.
7. Peacock O1, Speake W, Shaw A, Goddard A.Clostridium difficile enteritis in a patient after total proctocolectomy.BMJ Case Rep. 2009;2009.
8. Kim JH1, MuderRR.Clostridium difficile enteritis: a review and pooled analysis of the cases.Anaerobe. 2011 Apr;17(2):52-5.
9. Holmer C1, Zurbuchen U, Siegmund B, Reichelt U, Buhr HJ, Ritz JP.Clostridium difficile infection of the small bowel–two case reports with a literature survey.Int J Colorectal Dis. 2011 Feb;26(2):245-51
10. Wee B1, Poels JA, McCafferty IJ, Taniere P, Olliff J.A description of CT features of Clostridium difficile infection of the small bowel in four patients and a review of literature.Br J Radiol. 2009 Nov;82(983):890-5.
11. Kurtz LE, Yang SS, Bank S.Clostridium difficile-associated small bowel enteritis after total proctocolectomy in a Crohn’s disease patient.JClinGastroenterol. 2010 Jan;44(1):76-7.
12. Ishida Y1, Maegawa T, Kondo T, Kimura A, Iwakura Y, Nakamura S, MukaidaN.Essential involvement of IFN-gamma in Clostridium difficile toxin A-induced enteritis. JImmunol. 2004 Mar 1;172(5):3018-25.
