Study Bay Coursework Assignment Writing Help
Science versus Society
Introduction
Did the 1998 campaign to halt the rise of teen pregnancies contribute to the rise of the older mother in the 21st century?
Western cultures once frowned upon unmarried or teen mothers. These women had contributed to their own demise, in societies eyes, an early to mid-1900 view, when women’s rights were few economically politically or socially, women were marginalised.
In contrast, the 21st-century, woman in England has choices she has access to education and money and can develop a career but most importantly she can also choose when to start a family, she should feel be feeling empowered.
During the essay I will discuss the governments take on teenage pregnancies in 1998, IVF and the older mother, the optimal age to have a baby, the older mothers experience to that of a teen mum support and fertility.
Body
The age of sexual consent was set in 1885 at 16, mid-adolescence. Although they’ve been a few attempts to have this age reduced, it remains the same. In the mid 60’s the contraceptive pill was made available on the NHS to married women between 16- 49, it seems strange now to consider a girl of 16 being married let alone denying contraception to an over 49-year-old when she could still conceive. Life expectancy was roughly 71, maternal mortality had improved, due to advancement in medical hygiene and medicine, see Appendix 7.
Garrison.W.& Felice M.E. (2009), Outlined the various developmental stages of an adolescent. The term teen or adolescent in its self means a period of developing emotionally physically and mentally the process settling down between 18- 20 late adolescence.
In the mid-’90s, the Labour government was driven to implement a campaign to reduce teen pregnancies, as England was reported to having the highest rate of teen pregnancy within Europe, recognising that teen pregnancies within themselves were disadvantageous to women causing pernicious socioeconomic hardship generationally.
Teenage pregnancy’s peaked 1996 Skinner.S. R, Marino. J.L. (2016),
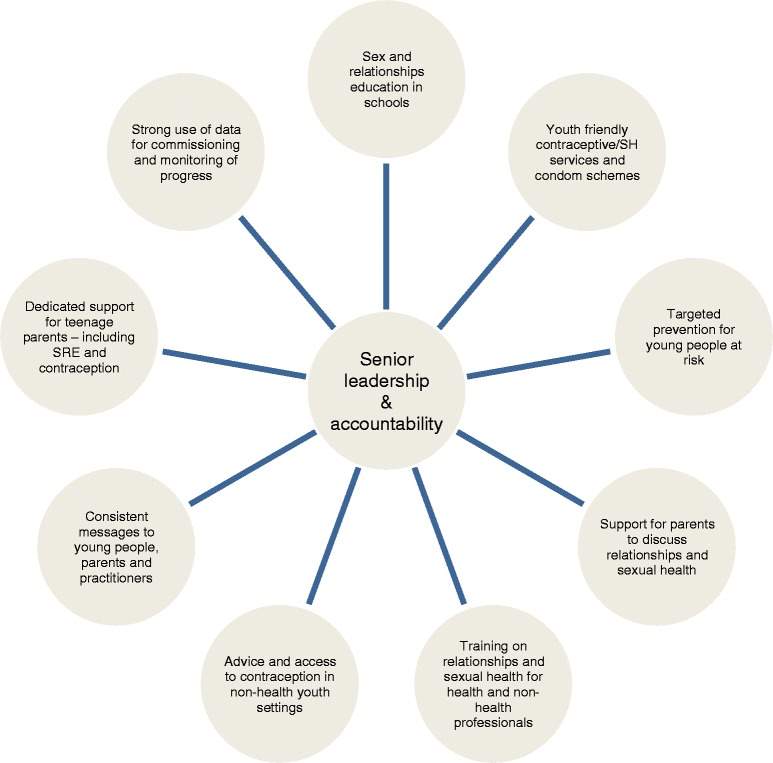
The government launched its campaign in 1998, the campaign would run for 10-years the focus group, being those below eighteen, Hadley. A Ingram. R & Chandra-Moil.V (2016). The campaign would work through a multi-agency approach see Appendix 3, mid-way through the campaign in 2005 an 11% success rate was recorded nationally with one local authority announcing a 43% success rate Skinner.S. R, Marino. J.L. (2016). By 2008 the teen pregnancy rates had declined by 13%. Frances. G. (2010), stated that had the 1998 intervention not been implemented births would have increased by 42,000 cumulatively. Conception continued to fall, reported in 2014 as 22,653, a reduction of 6.8%. Haines.N. (2017), see appendix 4. The multi-agency approach towards teen sexual education, open discussion and the availability of contraception appeared to be working.
Henig. R.M (2012). quoted Mirowsky. J, stating the best biologically age to have a baby as late adolescence the too early twenties, due to the body’s ability to reproduce peaking. Mirowsky. J. (2005), outlined that women who gave birth shortly after puberty were prone to experiencing health problems and that this was reduced if the first pregnancy happened up to and beyond 21 onwards.
Upon observing teens and twenty-somethings, of today, it’s hard to imagine this demographic on mass being parents to the next generation, the mental impact of having a baby on today’s teens cannot be underestimated. That being said there was the 90’s generation of teens who were parents.
Now in the 21st century, the proportion of 18-30-year olds living at home with their parents equal 32%. They are busy working, socialising and studying Relationships for them are different, Ofcom (2015), stated, Smart Phone usage at 90% between the 16-24-year olds, could the rise of Smartphone take some credit for the decline in the birth rate for the under the ’20s.
What’s known, is the younger the woman the more likely she is to experience health problems, it’s acknowledged that being biologically suitable for birth is out of kilter with societies norms Mirowsky. J.
The under 18 focus group of 1998-2008 would be in their late 30s to 40 + now, this demographic may have directly or indirectly been affected by the 1998 campaign, if the reports of the campaign’s success are to be believed, some of these women could be accounting for the rise in the older mother.
I have developed a narrative for the older IVF mother, she’s spent the last 20 years, building a career educating herself getting on the property ladder possibly waiting for the ideal opportunity to start a family with the right person, or not. The older professional woman has possibly spent many years managing her fertility with contraception using the 1960’s NHS model of a women’s choice that coupled with the 1998 campaign.
Once she no longer required contraception, her view shifted towards starting a family, time to get pregnant. However not every woman got pregnant immediately this was dependent on the type of contraceptive previously taken, it could take from 3 months to a year from stopping contraception to getting pregnant or to be deemed as requiring help.
This couldn’t be further from the experience of a teen who has possibly ignored contraception and conceived without trying.
With the optimal age to conceiving being between 21 and 34. The Office of National Static’s reported the highest rise in pregnancies to be in over 35 demographics, see Appendix 5. Mirowsky.J, stated that women over 35 started experiencing health problems, which begin to impact their fertility around at around 35.
There appears to be a window of 13 years, where the older woman can capitalise on the time of personal growth and empowerment. To possibly avoid the route of becoming an IVF mother, NHS (2017), stated 1in 7 couples experience difficulty conceiving.
Upon accepting that what should have been a natural process now requires a conversation with a third party, isn’t possibly what many women planned when aiming to become a parent.
The opposite can be said of teens, once pregnant some teens go into denial not reaching out for help, this state of denial can result in poor access to antenatal care. NHS [2010], Babies born to teens are more likely to be a pre-term pregnancy with low birth weight, with the teen at high risk of having high blood pressure, which can affect the kidneys, and be harmful to both baby and mother dependent on the mother’s adolescent age
Some of the symptoms being monitored by the Health Care professional for teens can also be seen in IVF mothers.
However, alongside the emotional and mental turmoil experienced by the older IVF mother, being described in these various ways, geriatric, older mother, when she’s only 35-40, would stop anyone in their tracks, or knowing that a medical condition she’d experienced could have had impacted on her conceiving, such as endometriosis or an STD. Finally, pregnant she’s pregnant, then she suffers a miscarriage and possibly another.
Fertility clinics work with women up to age 47, an additional 4 years beyond the NHS the number of women requesting IVF in 2018 was 60,000. This figure covered all circumstances requiring IVF including the older mother.
If a mother to decide to embark upon IVF through the NHS, the journey is are vast. The NSH will Help women under the ages of 43, cared for by their Helped conception unit, NHS (2018), To be accepted the IVF patient, has to of been actively trying to conceive for the past two years, although she has the option to choose the private route. Many blood tests later, the following steps must be covered
Step 1: suppressing the natural menstrual cycle,
Step 2: boosting the egg supply
Step 3: checking progress,
Step 4: collecting the eggs, Step
5: fertilising the eggs
Step 6: embryo transfer, a scan to check for success
NHS (2018)
The teen mum’s narrative, she expected to remain education complete the process up to year 11. The limitations are set by her, where her education is concerned. She can move on to university eventually.
Its acknowledged that after her first child the journey and route could possibly be harder, teen mums, are more likely to spend some time up until she’s 30 as a single mother she may even have added to her family with one more child. Although some teens will continue with their studies, while pregnant. This can come with an emotional and mental turmoil, on one hand, she knows she needs her education more than ever before, to provide for herself and her child however she has to go through her pregnancy in full view of her parents, her peers, their parents and teachers alike. This can add an additional layer of stress and anxiety.
The outline description of a teen’s pregnancies mental and emotional state mirrors that of a teenager developmentally, mood swings, depression, difficulty concentrating, anxiety, sadness, difficulty sleeping
Women who conceived through IVF reported the following emotions, frustration, isolation and emotionally exhausted.
Conclusion:
In discussing the teenage mother and 1998 campaigned to reduce teen pregnancies as its blighted UK society, I acknowledged that the government noted it as harmful to both mother and child generationally.
However, following Mirowsky.J, findings around the biological age versus the optimal and society for having the first child, although 1998 campaign was successful, it may have benefited from being aimed at a higher adolescent group, this could have given a higher success rate earlier into the campaign. Upon implementing the campaign, there was no precursor to looking ahead at the knock-on effect within 10 -20 years, the aim was met. It may have worked better had the legal age of consent been implemented alongside the campaign.
Focusing on the under 18’s was contradictory to Mirowsky.J, optimal age, and even the upper adolescent age. The 1998 campaign focused on the group that would be at risk. This action could have contributed to the rise of the older mother, who has been more focused on building a career, directly or indirectly conform to societies norms in line with a developing country view.
I concluded that what the older career mother hadn’t built into her plan, was her ability to conceive naturally, after years of managing her own fertility exercising her choice feeling empowered in doing so. Her choice to conceive naturally had narrowed forcing her to acknowledge that the empowerment that contraception had afforded, had also reduced her choices too, IVF, surrogacy, adoption or to remain childless.
I focused on IVF older mother. In comparing the older professional IVF mother to teen mothers, what stood out was timing it appeared to be a key factor.
There were times within each of their lives when each could have benefited from what the other had. The teen mother, money and education and time to develop more, the older mother the ability to conceive naturally without the need for IVF, to turn the clock back to a time-optimal to conceive. For both sets of women, timing was a key factor.
Both sets of women were considered high risk, mirroring each other’s risk factors at times. The older IVF mother’s antenatal care intense and intrusive, resulting in her conforming to health care professionals request, possibly conforming based on the journey to conceive and the relationship that been established, with the health care team. For some women her confirmative manner would have been built upon with anxiety, which intern reduces her empowered demeaner, bringing forth complicity and acceptance. Which can possibly work against her. The teen however also high risk may not have had the same level of interaction with the healthcare professionals, is less likely to be induced or to be given a caesarean.
When facilitating, I’d like to empower women to trust in themselves, I’d like the older IVF mother not to feel pressured into being induced based on her age or the methods in which she conceived. Outlining the acronym B.R.A.I.N, Benefits, Risk, Alternative, Intuition, Now/Nothing noted by Reed.R (2018).
As a teen mother and older mother, I straddle both of these timelines, see Appendix 2, while not openly attaching their experience to myself, I feel I’ll able to show empathy and congruence.
Being a first-time mother is a time filled with anxiety regardless of age, have the journey of IVF can be a major factors in how the mother feels at the end of her journey, anything the health care professionals suggest or advise the mother will be willing to oblige, although she may well be aware of B.R.A.I.N, her ability to apply it may be hard. However, having the knowledge informs choice.
Both groups of women are susceptible to postnatal depression, possibly brought about by transition and acceptance and change both will require support, the teenager will be going through developmental changes, that coincide with the hormonal changes encountered during Pre and postnatal pregnancy. The IVF older mother will also have been exposed to additional hormones to Help the conception.
Support for the teens is usually given by family, extended and immediate alongside friends and external agencies. This forms a part of the support network all of them pulling together to create the village environment needed, to ensure a positive outcome. The mutual consent being, she needs all the support because she’s only a child, or she young based upon her age, this relationship can help a teen to exist in the PAC model of development see Appendix 8, where the learning style with the new responsibility moves in and out of their role as parent, to child, and sometimes adult, although the teen may not recognise this. My role as a practitioner will be to respect the client, engaging with them as a young adult, speaking to them in an age appropriate manner. As the teen becomes a mother, she straddles two entities. The teens struggle with transition is different two that of a woman who is pressed pause on her career. The teen cannot press pause, she has no choice but to go through the remainder of her development process
The older IVF mother possibly requires the same level of support however based on her age, it will not be available in the same manner unless paid for.
For this reason, I would plant seeds, within the session to encourage the development of support network, signposting and reinforcing the benefits of being a part of groups. McMahon. M (2018), spoke about the camaraderie gained from being a part of a group and how this has been broken down with in the UK. What neither mother was aware of, is how venerable she is and how relentless and lonely it can be as a first-time mum.
Both sets of women are experiencing firsts, however due to the built-in support the teen receives she may never really understand, that being said many teen mums speak of isolation even with the support. The teen maybe calling it isolation, but it could be the grieving of adolescence. Being a mum can bring restrictive constraint. As I think about the journey for a teen mum it’s harsh.
References
- Frances.G. 2010.Teenage Pregnancy Independent Advisory Group [Online]. [Accessed 22 January 2019]. Available from:
- https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/181078/TPIAG-FINAL-REPORT.pdf
Garrison.W & Felice.M.E 2009. Books.Google.co.uk [Online]. [Accessed 25 January2019]. Available from:
- https://books.google.co.uk/books?hl=en&lr=&id=OlWaMWGS01AC&oi=fnd&pg=PP1&dq=Adolescence+by+william+Garrison+and+marianne+e.Felice&ots=YRE16SB_H5&sig=jIeoPUHCOXm3R6fyY_iRIbNkKbs#v=onepage&q=Adolescence%20by%20william%20Garrison%20and%20marianne%20e.Felice&f=false
- Hadley.A, Ingram. R & Chandra-Moli.V 2016. NCBI [Online]. [Accessed 22January 2019]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5120422/
- Haines.N. 2017. Office of National Statics website [Online]. [Accessed 22 January 2019]. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/conceptionandfertilityrates/bulletins/conceptionstatistics/2014
Henig. R.M 2012. Psychology Today Website. [Online]. [Accessed 24 January 2019]. Available from:
- https://www.psychologytoday.com/us/blog/cusp/201211/whats-the-best-age-have-baby
- McMahon. M (2018), Why Mothering Matters. London. Pinter and Martin Ltd.
- Mirowsky, J. (2005). ‘Age at First Birth, Health, and Mortality’. Journal of Health and Social Behavior, 46(1), pp.32-50.
- Reed.R (2018). Why Induction Matters. London. Pinter and Martin Ltd.
- Rudgard. O 2018. Telegraph Website. [Online]. [Accessed 25th January 2019]. Available from: https://www.telegraph.co.uk/news/2018/03/27/older-mothers-rise-over-40s-become-group-rising-conception-rate/
- Skinner.S.R, Marino. J.L. 2016. Lancet Website. [Online]. [Accessed 22 January 2019]. Available from: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(16)30589-X/fulltext
- Ofcom 2015. UK now a smartphone society Website. [Online]. [Accessed 22 January 2019]. Available from: https://www.ofcom.org.uk/about-ofcom/latest/features-and-news/uk-now-a-smartphone-society
- NHS [2018] NHS Website. [Online]. [Accessed 27th January 2019]. Available from:https://www.nhs.uk/conditions/ivf/what-happens/
- NHS [2017] NHS Website. [Online]. [Accessed 27th January 2019]. Available from:https://www.nhs.uk/conditions/infertility/
- NHS [2010] NHS Website. [Online]. [Accessed 27th January 2019]. Available from:https://www.nhs.uk/news/pregnancy-and-child/birth-complications-for-teen-mums/
Bibliography
- Writings from Hackney Reading Centre. (1980). Every Birth It comes Different: London. Centreprise.
Appendix 1
Reflection Entry 3 12 Nov 2018: Course Observation:
My feeling about the observation were mixed. There I was observing a fast tract ANT session being run over 12 hours following the same format that I cover for Essentials with a slant on statically based information. I realised in that moment that I already had most of the tools required to be an ANT practitioner, I really needed to build upon my own knowledge base and my ability to retain information, so that I could impart in a fun-filled activity led manned.
I don’t feel any differently now than I did at the time of observing. I wish I’d got on board earlier, with building my knowledge bank.
I have since re-evaluate my current Essentials Session plans. Literally cutting it up and reset it in a different way, so it flows.
I’ve reorganised my facilitating material to reflect the new class plan.
I ran a new group last weekend, I was so happy with my own delivery. I’d even set up a Padlet, to give the polished professional appearance I’d wanted to do for so long, but lacked due to not putting in the time to learning how to use the APP
Where I know I need help is in differentiating an ANT class from an Essentials Class, the only difference being that during an Essentials session Breastfeeding advice is offered.
From this point on, I intend to develop my knowledge base, I believe I will struggle in offering anything other than the quality information I’d gathered regardless of the class title. I would need to discuss this aspect with the PSA or with an assessor.
I struggle to retain facts, so I will be developing some flash cards using words and images to reinforce my knowledge retention. I will also practice speaking out loud, so I can build my confidence.
I’ll know I’m different in clinical practice by the way in which I’m able to answer client’s questions, I would no longer use the stock response of, I’ll come back to you, in instances where currently I genuinely don’t know the answer.
The main things I’d taken away from this experience. Was that I was lacking in knowledge. I need to be permanently in learning mode, as things always change. It’s good to get out there and see what others are doing.
I was also able to share a few activities with the practitioner. She also made me feel more confident in asking the groups to move around and to take part in activities I’d arranged for them.
Appendix 2
Reflection Entry 01 Oct 2018
As I sat to reflect on my own experience of birth, I struggled to remember the finer details, was it half an hour or possibly an hour and a half of pushing, did I refuse to push through fear of the unknown, did I swear was there a sense of tension or anxiety in the labour room. Did I feel love and appreciation from my partner? I remembered the last hour leading up to the birth and most defiantly the hours after. I remember starting off with one midwife, and then I had two. At the point of actual pushing there was a lot of praises, “you’re doing really well,” from one, “ keep pushing,” from the other, “you can do this” and some direction, “ok, I just want you to slow down your pushing and just pant”, another instruction “can you just adjust yourself, come towards the end of the bed”.
Upon reflection, I recall that my discomfort and feelings about the contractions changed during the process of giving birth, to that of labouring, I was no longer focused on the pain. I don’t believe I remember giving birth as a painful process, I do remember being told “I want you to use the contractions” and boy did I gripped the gas and air at one point and then the mattress and my sister’s arm and I pushed. I was so very focused on the midwives, they became my coaches, I no longer cared about my partner or my sisters’ voices or input they were background noise. Upon Assessment at the immediate point of birth, I’d put all my trust into the midwives listening out for their every instruction.
I’m unsure how my actual birth experience will affect my facilitation as a practitioner, I have however concluded that women who decide to have a hospital birth, have already opted to have help and Helpance in one form or another. All labouring women will benefit from a woman to woman input during labour as will birth partners especially those who are fortunate to encounter a male midwife. The attending midwife may or may not have a personal experience or understanding of what the birthing woman’s going through. What she will have is the expertise, experience and knowledge to step up to help and Help a birthing woman, being gentle, encouraging or firm in equal measure where required. I feel confident in saying view your midwife as your coach, she there to look after you and your baby, a labouring/birthing woman needs to work with the midwife.
During my facilitation, I’d like to empower and impart knowledge, I feel it can be empowering for a birthing mother to know what’s happening to her body and why the process of knowing may even bring a sense of calm to a birthing mother.
Appendix 3
Hadley.A, ngram. R & Chandra-Moli.V (2016)
Appendix 4 Hadley. A, Ingram. R & Chandra-Moil (2016) Haines.N. (2017)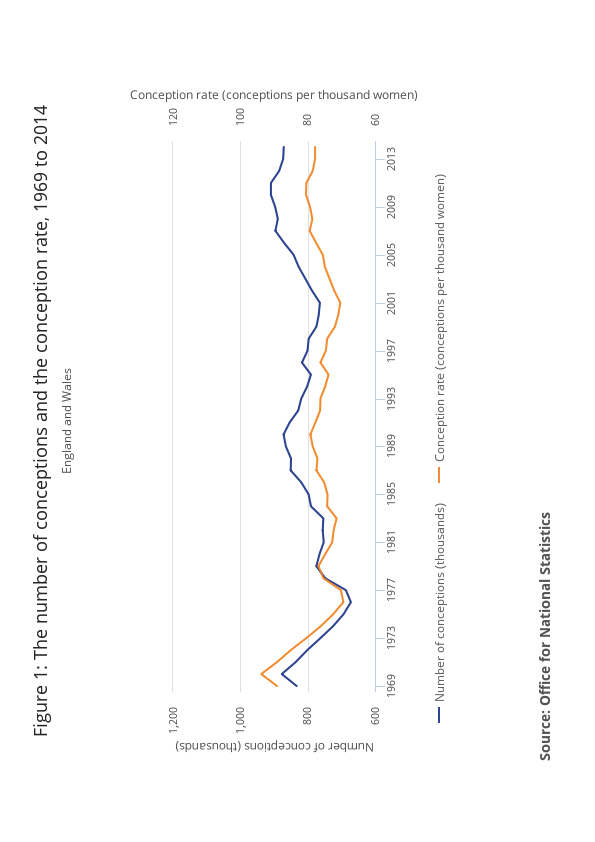
Appendix 5