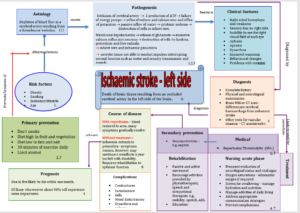
Sample Concept Map: Stroke
Sample Assignment:
Topic: Left Sided Heart Failure Concept Map
Left Sided Heart Failure Concept Map. The Map should be about Left-Sided Heart Failure
Below are the Sub-heading that needs to be in the Concept Map.
Disease
Definition
AETIOLOGY
PATHOGENESIS
PATHOGENESIS
DIAGNOSIS
TREATMENT
COURSE OF DISEASE
PROGNOSIS
PREVENTION
· The separate Reference page for Concept Map. You may have more than 2 reference
· Visually Stimulating, add pictures in the background and visually attractive. Below is an sample example but this concept map needs to look unique and visually very appealing, please.
· Add pictures of heart, lungs what ever connects to the Map and its information.
· I have attached a sample of the concept map of another topic to guide you what information requires in the map.
· 500 words and it is worth 25 Marks.
Please see attach other files for questions and Marking Criteria.
Disease: Left-sided heart failure
Definition: Left-sided heart failure, also known as left ventricular failure, occurs when the left ventricle becomes unable to pump a sufficient amount of blood to the body’s tissues (Mayo Clinic, 2022).
AETIOLOGY: Common causes of left-sided heart failure include coronary artery disease, hypertension, previous heart attack, cardiomyopathy, and valvular heart disease (American Heart Association, 2023).
PATHOGENESIS: Over time, one of the above conditions can weaken and damage the muscle of the left ventricle, impairing its ability to contract effectively. As a result, blood backs up in the lungs and veins as the heart struggles to pump forward (NHS, 2018).
DIAGNOSIS: Diagnosis involves physical exam, medical history, echocardiogram, electrocardiogram, chest x-ray, and blood tests such as BNP or NT-proBNP levels. Symptoms include shortness of breath, fatigue, swelling of legs/ankles, rapid or irregular heartbeat (Mayo Clinic, 2022).
TREATMENT: Treatment focuses on managing symptoms, improving cardiac function, and preventing hospitalization. This may include diuretics, ACE inhibitors, beta blockers, ARBs, aldosterone antagonists, digoxin, and device therapies as needed (American Heart Association, 2023).
COURSE OF DISEASE: With treatment, the condition can often be managed successfully. However, it may progress to more severe symptoms over time if risk factors are not controlled (NHS, 2018).
PROGNOSIS: Prognosis depends on the underlying cause and how well the condition is managed. Following treatment guidelines closely can help prevent hospitalizations and support a good quality of life (Mayo Clinic, 2022).
PREVENTION: Maintaining a healthy lifestyle, controlling risk factors like high blood pressure and diabetes, and adhering to medication can help prevent the initial onset or progression of left-sided heart failure (American Heart Association, 2023).
####
______________________________
Example 2
Scenario
You have already learned about evidence-based practice and quality improvement initiatives in previous courses. You will use this information to guide your assessments, while also implementing new concepts introduced in this course. For this assessment, you will engage in the Vila Health: Using Concept Maps for Diagnosis scenario, develop a concept map, and provide supporting evidence and explanations.
Engage with a Vila Health scenario and then create a concept map that illustrates a plan for achieving high-quality outcomes for a patient.
Introduction
Note: Each assessment in this course builds on the work you completed in the previous assessment. Therefore, you should complete the assessments in this course in the order in which they are presented.
The biopsychosocial (BPS) approach to care is a way to view all aspects of a patient’s life. It encourages medical practitioners to take into account not only the physical and biological health of a patient, but all considerations like mood, personality, and socioeconomic characteristics. This course will also explore aspects of pathophysiology, pharmacology, and physical assessment (the three Ps) as they relate to specific conditions, diseases, or disorders.
The first assessment is one in which you will create a concept map to analyze and organize the treatment of a specific patient with a specific condition, disease, or disorder.
The purpose of a concept map is to visualize connections between ideas, connect new ideas to previous ideas, and to organize ideas logically. Concept maps can be an extremely useful tool to help organize and plan care decisions. This is especially true in the biopsychosocial model of health, which takes into account factors beyond just the biochemical aspects of health. By utilizing a concept map, a nurse can simplify the connection between disease pathways, drug interactions, and symptoms, as well as between emotional, personality, cultural, and socioeconomic considerations that impact health.
Professional Context
The purpose of a concept map is to visualize connections between ideas, connect new ideas to previous ideas, and to organize ideas logically. Concept maps can be an extremely useful tool to help organize and plan care decisions. This is especially true in the context of the biopsychosocial model, which takes into account factors beyond just the biochemical aspects of health. By utilizing a concept map, a nurse can simplify the connection between disease pathways, drug interactions, and symptoms, as well as between the emotional, personality, cultural, and socioeconomic considerations that impact health.
Scenario
You have already learned about evidence-based practice and quality improvement initiatives in previous courses. You will use this information to guide your assessments, while also implementing new concepts introduced in this course. For this assessment, you will engage in the Vila Health: Using Concept Maps for Diagnosis scenario, develop a concept map, and provide supporting evidence and explanations.
Instructions
For this assessment, you will develop a concept map and a short narrative that supports and further explains how the concept map is constructed. The bullet points below correspond to the grading criteria in the scoring guide. Be sure that your evidence-based plan addresses all of the bullet points. You may also want to read the Concept Map scoring guide and Guiding Questions: Concept Map [DOCX] to better understand how each grading criterion will be assessed.
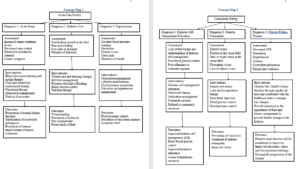
Part 1: Concept Map
Develop an evidence-based concept map that illustrates a plan for achieving high-quality outcomes for acute and chronic stages for a patient with renal failure related to diabetes in both an acute care facility and in the community.
You can achieve this by following the Vila Health scenario.
You will have a total of two concept maps. One will show the acute care facility with three diagnoses, and the other will show a home health community setting with three diagnoses.
Part 2: Additional Evidence (Narrative)
Justify the value and relevance of the evidence you used as the basis for your concept maps.
Analyze how interprofessional strategies applied to the concept map can lead to the achievement of desired outcomes.
Construct the concept maps and linkage to additional evidence in a way that facilitates a reader’s understanding of key information and links. This will be done by adding links in each section of the concept map that will show your value, relevance, and evidence.
Integrate relevant sources to support assertions, correctly formatting citations and references using current APA style.
Submission Requirements
Length of submission: Each concept map should be on a single page, if at all possible. You will add links to each section of your concept map for additional evidence and narratives that support your concept maps.
Number of references: Cite a minimum of 3–5 sources of scholarly or professional evidence that support your concept map, decisions made regarding care, and interprofessional strategies. Resources should be no more than five years old.
APA formatting:
For the concept map portion of this assessment, format resources and citations according to current APA style. Please include references both in-text and in the reference page that follows your narrative.
For the narrative portion of this assessment: An APA Template Tutorial [DOCX] is provided to help you in writing and formatting your analysis. You do not need to include an abstract for this assessment.
Competencies Measured
By successfully completing this assessment, you will demonstrate your proficiency in the following course competencies and scoring guide criteria:
Competency 1: Design patient-centered, evidence-based, advanced nursing care for achieving high-quality patient outcomes.
Develop an evidence-based concept map that illustrates a plan for achieving high-quality outcomes at the acute and chronic stage for a patient with renal failure related to diabetes in both an acute care facility and in the community.
Justify the value and relevance of the evidence used as the basis for a concept map.
Competency 4: Evaluate the efficiency and effectiveness of interprofessional care systems in achieving desired health care improvement outcomes.
Analyze how interprofessional strategies applied to the concept map can lead to achievement of desired outcomes.
Competency 5: Communicate effectively with diverse audiences, in an appropriate form and style, consistent with organizational, professional, and scholarly standards.
Create links within each section of the concept map for any additional evidence in a way that facilitates understanding of key information.
Integrate relevant sources to support assertions, correctly formatting citations within the concept map and references using current APA style.
You are an ICU nurse (black male) at St. Anthony Medical Center. You have been assigned Mrs. Smith (black female), a 52-year-old with a history of Type II Diabetes Mellitus, who was admitted this morning with high glucose levels and Acute Renal Failure.
Ask her some questions in order to create a concept map.
Mrs. Smith
I see that your HA1C is at 8.5. Can you give me a history of your blood glucose readings over the last 2 weeks?
Hide Response
Mrs. Smith: My fasting blood sugars have been running around 200 with it getting as high as 350+ after each meal. I can tell that I wasn’t feeling very good, and I am swelling in my legs more than usual. I also have some blurred vision and I am very tired.
Are you experiencing any other symptoms?
Hide Response
Mrs. Smith: Yes, I think so but I’m not sure if they are related.
What are some of the other things going on?
Hide Response
Mrs. Smith: I have not voided as often as before, and I feel a little short of breath when I get up to walk to the mailbox. I also feel weak and even a little nauseous.
Optimizing Outcomes for Patients with Diabetes and Chronic Kidney Disease through Interprofessional Strategies
Introduction
Diabetes is a leading cause of chronic kidney disease (CKD) worldwide. Having both diabetes and CKD significantly increases the risks of kidney failure, cardiovascular disease, and premature death. Effective management requires a comprehensive approach to control blood sugar and other risk factors through lifestyle modifications, medications and coordinated care. Interprofessional collaboration between healthcare providers has been shown to improve outcomes for patients with complex chronic conditions.
Search Results
A review of current literature found several references highlighting the importance of interprofessional care models. A consensus report by the American Diabetes Association and Kidney Disease Improving Global Outcomes emphasized the need for a team-based approach involving physicians, nurses, dietitians and pharmacists (1). Another source discussed the roles of primary care doctors, nurses and pharmacists in providing coordinated care, education and monitoring patients in the community setting (2). A third reference examined the impact of pharmacist involvement in interprofessional teams on managing patients with chronic diseases (3).
Discussion
The references demonstrated several best practices for interprofessional management of diabetes and CKD:
Comprehensive, evidence-based care plans developed jointly by multidisciplinary teams including physicians, nurses, pharmacists and other providers.
Regular monitoring and communication between all providers to ensure holistic care addressing medical, nutritional and psychosocial needs.
Structured patient education from various team members to promote effective self-management and symptom recognition.
Care coordination in the community setting through collaboration between primary care, nursing and pharmacy services.
Interprofessional strategies can optimize treatment and reduce risks of complications or hospital readmissions.
In summary, the literature review supports adopting interprofessional approaches emphasizing team-based care and active patient involvement to significantly improve outcomes for those with diabetes and CKD. Collaborative models align with providing high-quality educational materials on managing these complex chronic conditions. Further research can help refine interprofessional strategies and close remaining knowledge gaps.
References
De Boer, I. H., Khunti, K., Sadusky, T., Tuttle, K. R., Neumiller, J. J., Rhee, C. M., Rosas, S. E., Rossing, P., & Bakris, G. (2022). Diabetes management in chronic kidney disease: A consensus report by the American Diabetes Association (ADA) and kidney disease: Improving global outcomes (KDIGO). Diabetes Care, 45(12), 3075–3090. https://doi.org/10.2337/dci22-0027
National Kidney Foundation. (2022, May 25). Managing blood sugar for kidney health. National Kidney Foundation. Retrieved April 29, 2023, from https://www.kidney.org/atoz/content/managing-blood-sugar-for-kidney-health
Rahayu, S. A., Widianto, S., Defi, I. R., & Abdullah, R. (2021). Role of pharmacists in the interprofessional care team for patients with chronic diseases. Journal of Multidisciplinary Healthcare, Volume 14, 1701–1710. https://doi.org/10.2147/jmdh.s309938
